Publications
Preprints
2002
Homing and repopulation of nonobese diabetic/severe combined immunodeficient (NOD/SCID) mice by enriched human CD34+ stem cells from cord blood, bone marrow, or mobilized peripheral blood are dependent on stromal cellderived factor 1 (SDF-1)/CXCR4 interactions. Recently, human cord and fetal blood CD34+CD38-CXCR4- and CXCR4+ cells, sorted with neutralizing anti-CXCR4 monoclonal antibody (mAb), were shown to have similar NOD/SCID repopulation potential. Herein we report that human cord blood CD34+CXCR4+ (R4+) and CD34+CXCR4- (R4-) subsets, sorted with neutralizing anti-CXCR4 mAb, engrafted NOD/SCID mice with significantly lower levels of human cells compared with nonsorted and SDF-1-migrated CD34+ cells. Coinjection of purified cells with 10 μg anti-CXCR4 mAb significantly reduced engraftment of all CD34+ subsets, and 50 μg completely abrogated engraftment by R4- and CD34+ cells. Importantly, R4- cells harbor intracellular CXCR4, which can be rapidly induced to cell surface expression within a few hours. Moreover, 48 hours of cytokine stimulation resulted in up-regulation of both cell surface and intracellular CXCR4, restoring migration capacities toward a gradient of SDF-1 and high-level NOD/SCID repopulation potential. In addition, homing of sorted R4- cells into the murine bone marrow and spleen was significantly slower and reduced compared to CD34+ cells but yet CXCR4 dependent. In conclusion, R4- cells express intracellular CXCR4, which can be functionally expressed on the cell membrane to mediate SDF-1-dependent homing and repopulation. Our results suggest dynamic CXCR4 expression on CD34+ stem and progenitor cells, regulating their motility and repopulation capacities.
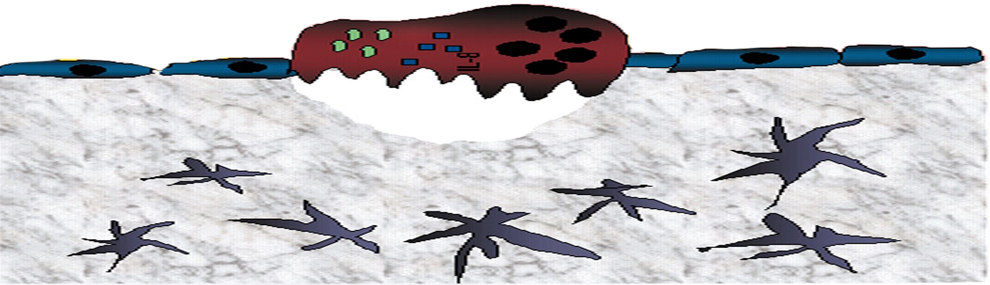
Hematopoietic stem cells are identified based on their functional ability to migrate via the blood circulation of transplanted recipients, to home to the host bone marrow and to durably repopulate this organ with high levels of maturing myeloid and lymphoid cells. While a small pool of undifferentiated stem cells with the potential to repeat the entire process in serially transplanted recipients is maintained within the bone marrow, maturing cells are continuously released into the circulation. In recent years pre-clinical, functional in vivo models for human stem cells have been developed, using immune-deficient mice or pre-immune, fetal sheep as recipients. The mechanism of human stem cell migration, homing and repopulation in transplanted immune-deficient NOD/SCID and NOD/SCID/B2mnull mice as well as the accessory mediators that facilitate these processes, will be reviewed. In particular, the essential roles of the chemokine SDF-1 and its receptor CXCR4 which mediate and regulate stem cell homing and repopulation will be discussed.
Mobilization of hematopoietic stem and progenitor cells from the bone marrow into the circulation by repetitive, daily stimulations with G-CSF alone, or in combination with cyclophosphamide, is increasingly used clinically; however, the mechanism is not fully understood. Moreover, following mobilization stem cells also home back to the bone marrow, suggesting that stem cell release/mobilization and homing are sequential events with physiological roles. Previously, a role for cytokines such as G-CSF and SCF, and adhesion molecules such as VLA-4 and P/E selectins, was determined for stem cell mobilization. Recent results using experimental animal models and samples from clinical mobilization protocols demonstrate major involvement of chemokines such as stromal derived factor-1 (SDF-1) and IL-8, as well as proteolytic enzymes such as elastase, cathepsin G, and various MMPs in the mobilization process. These results will be reviewed together with the central roles of SDF-1 and CXCR4 interactions in G-CSF or G-CSF in combination with cyclophosphamide-induced mobilization. Furthermore, the central role of this chemokine in stem cell homing to the bone marrow as well as retention of undifferentiated cells within this tissue will also be discussed.