Biomedicine and beyond
Achievements of the Grand Israel National Center for Personalized Medicine
Features

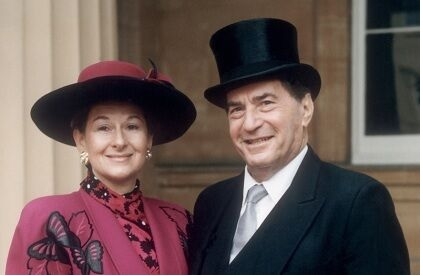
The Nancy and Stephen Grand Israel National Center for Personalized Medicine was founded in 2012 with a goal to bring together a diverse group of scientific talents under one roof and to equip them with the cutting-edge tools needed to move medicine forward. It came to life thanks to major support from Nancy and Stephen Grand of San Francisco and other visionary donors.
Initiated by the Weizmann Institute, the Grand Center (also known as the G-INCPM) was designed to create a national resource where all of Israel’s biomedical researchers could collaborate with teams of experts to advance the basic research needed to create new drugs and therapeutic approaches for treating and curing diseases. These areas of expertise are divided into the Grand Center’s four “pillars”: the Crown Genomics Institute, the de Botton Protein Profiling Institute, the Ilana and Pascal Mantoux Bioinformatics Institute, and the Maurice and Vivienne Wohl Drug Discovery Institute. The Wolfson Family Charitable Trust of the UK gave a visionary gift to support the renovation and construction of the former Solar Tower, which now houses the G-INCPM. Rounding out the Grand Center’s institutional resources are the Shapell Institute—which supports IT infrastructure—and the Institute for Medicinal Chemistry.
The result is a fully integrated enterprise that harmonizes the essential functions needed to speed up the translation of scientific discovery from the lab into the clinical arena.
Now celebrating its fifth anniversary, the Grand Center boasts an outstanding level of productivity, with 596 projects completed in 2017— a 20 percent increase over the total projects completed the previous year, and continuing the trend of rapid year-over-year growth that has characterized this Center since its inception.
The Center’s growing impact is seen in an important benchmark reached this year, with the number of projects completed in collaboration with scientists and clinicians outside of the Weizmann Institute (333) exceeding the number of projects performed with Weizmann collaborators (268). During 2017, Grand Center experts collaborated with researchers at the Hebrew University of Jerusalem, Bar-Ilan University, Tel Aviv University, the Technion, Ben-Gurion University of the Negev, the University of Haifa, and other institutions. Additional work paired Grand Center scientists with medical professionals at Sheba, Ichilov, Hadassah, Rabin and Barzilai Medical Centers.

Stephen and Nancy Grand
Pillars of progress
Many projects begin at the Crown Institute for Genomics, which facilitates the discovery of genomic indicators of disease risk. Activities at the de Botton Institute for Protein Profiling have doubled over the past year, in part a reflection of the acquisition of a key instrument that enables faster and more sophisticated analysis than is possible using the Institute’s previously available proteomic platforms. At the Mantoux Institute for Bioinformatics, experts use sophisticated algorithms and other techniques to sift through and make sense of reams of biological and medical data.
At the Maurice and Vivienne Wohl Institute for Drug Discovery, experts screen hundreds of thousands of chemical compounds as potential therapies using high-throughput systems. And this work just became more efficient, thanks to a new robotic system that has doubled the speed at which compounds can be delivered into well plates for screening and follow-up analysis. In addition, a new vial-handling robot will soon be installed to streamline the use of compounds synthesized in medicinal chemistry experiments. Also at the Wohl Institute, a new screening system—based on wide-field and confocal microscopy—is improving the Grand Center’s ability to analyze everything from cells to complex, multi-layered specimens.
Advancing personalized medicine
The need for cooperation between institutions in Israel is as necessary today as it was when the Center opened its doors in 2012, says Dr. Berta Strulovici, the Grand Center’s founding director. “An estimated 90 percent of top-selling, so-called ‘blockbuster’ medicines only work for 30 to 50 percent of patients, and adverse reactions caused by this ‘imprecise medicine’ account for about a third of acute hospital admissions every year,” she says. “There is a clear need for more personalized approaches, and that’s what our collaborative work at the G-INCPM is meant to accomplish.”
Dr. Strulovici is retiring from her position as Director at the end of this year.
The Center’s founding Steering Committee chair, Prof. Aaron Ciechanover—a biologist and Nobel Laureate from the Technion—also stepped down recently, passing the baton to another outstanding Israeli scientist, Prof. Chaim Cedar of the Hebrew University. Prof. Cedar is best known for his pioneering work that revealed the existence of DNA methylation, a fundamental mechanism that regulates which genes are turned on, and turned off, in every tissue of the body. His studies, conducted with Prof. Aharon Razin, have had a major impact in the fields of developmental biology, control of gene expression, epigenetics and cancer research.
“The G-INCPM is unique in the way it streamlines cooperation between the many different types of scientists working to clarify the molecular basis of health and disease,” Prof. Cedar says. “As a national resource, it empowers Israeli researchers, helping them generate comprehensive genomic data, which can be integrated into next-generation drug design and personalized therapeutics.”
Defeating cancer recurrence
In one recent project, scientists at the G-INCPM’s de Botton Institute for Protein Profiling teamed up with clinical experts from the Department of Neurosurgery at Jerusalem’s Shaare Zedek Medical Center to identify proteins involved in the recurrence of a cancer of the central nervous system known as malignant meningioma.
A meningioma is a tumor that forms on membranes that cover the brain and spinal cord, just inside the skull. Many meningiomas produce no symptoms and require no treatment. Malignant meningiomas, on the other hand, are treated either with radiation or surgery. However, up to 20 percent of such meningiomas recur—with three percent re-emerging in a malignant form. In some patients, tumors reappear a few months after the completion of treatment; in others, recurrence is delayed for five years or more.
The Shaare Zedek and G-INCPM teams successfully identified protein biomarkers associated with those patients likely to suffer swift recurrence of malignant meningioma, as well as late recurrence. In the future, these findings could help clinicians sharpen their diagnosis and strategize treatment, by identifying the quick-relapse patients who would most benefit from immediate radiotherapy, as well as others likely to have slower recurrence, and for whom radiotherapy’s side effects might outweigh its benefits.
Treating Louis-Bar syndrome
Another recent project, spearheaded by Tel Aviv University scientists and experts at the G-INCPM’s Wohl Institute for Drug Discovery, set out to identify compounds capable of correcting a defect in the mutant form of a gene called ATM—a defect associated with a serious autoimmune disease called Ataxia-telangiectasia, or A-T.
Also known as Louis-Bar syndrome, A-T is a rare, neurodegenerative syndrome that causes severe disability. Its symptoms, which can appear in early childhood, include impaired coordination and cognitive development, a weakened immune system, and damage to the body’s DNA repair mechanisms—something that increases the risk of cancer.
The collaborating scientists established a high-throughput screening protocol—testing thousands of molecules—to identify compounds that correct a splicing defect in the ATM gene. Several “hits” were identified, and are now being investigated in cells—an important step toward determining whether drugs based on these compounds have true therapeutic potential.
Individualized breast cancer treatment
In a promising study on breast cancer, researchers from Sheba Medical Center and Tel Aviv University partnered with the G-INCPM to identify possible strategies for personalized treatment for individual breast cancer patients, based on the changing gene expression patterns that underlie tumor progression and response to therapy.
Tracking 33 women being treated for breast cancer, Sheba clinicians collected tissue samples of three types: a tumor biopsy at the time of diagnosis, a sample of the surgically removed tumor tissue, and an additional sample of non-cancerous tissue adjacent to the tumor site. These samples will undergo a full proteomic analysis at Tel Aviv University, after which experts from the Grand Center’s Mantoux Institute for Bioinformatics will integrate the data, in order to link gene expression patterns with specific clinical outcomes.
This project is expected to aid in the development of diagnostic tools, as well as in the identification of genetic profiles associated with resistance to particular types of anticancer therapy.
Accurately predicting AML
Acute myeloid leukemia (AML) is characterized by an accumulation of mutations in hematopoietic (blood forming) stem cells. However, using this insight to predict AML onset is complicated by the fact that, as they age, healthy individuals also accumulate hematopoietic stem cell mutations.
Now, in a project performed in collaboration with the Grand Center’s Crown Genomics Institute and Assuta Medical Center, Dr. Liran Shlush of the Weizmann Institute’s Department of Immunology has developed a way to differentiate between individuals at high risk of developing AML and those with benign mutational activity.
Studying the blood cells of 95 individuals who later developed AML, Dr. Shlush and his G-INCPM colleagues performed deep sequencing of genes that repeatedly appeared in a mutated form. The overall mutational profile of these patients was shown to be distinct from control samples taken from healthy patients.
The genetic parameters revealed by Dr. Shlush’s study were used to create a model that accurately predicted AML-free survival. This model, which can identify pre-AML risk many years prior to disease onset, could in the future potentially be used in the clinic for earlier detection, disease monitoring, and therapeutic intervention.
Activities taking place at the Grand Center are fulfilling the mission articulated at its founding: to quicken the pace at which scientific discoveries can be transferred from bench to bedside.
“In five years of growth and highly productive interdisciplinary collaboration, this vision has become a day-to-day reality and we are moving toward better, more personalized patient care.”

The Wolfson Family Charitable Trust of the UK gave a magnanimous gift for the renovation and construction of the Grand Israel National Center for Personalized Medicine, formerly the Solar Tower.
Investing in Israel’s future
The Nancy and Stephen Grand Israel National Center for Personalized Medicine was never an abstract commitment for the philanthropists behind the name. That’s because the Grands, who live in San Francisco, personally experienced how cutting-edge biomedical science can save lives—specifically, Stephen’s own life.
“Many years ago, I was diagnosed with a fatal blood cancer called multiple myeloma, and was given two years to live,” he says. “At the same time, a new drug for this condition had just been approved. After a few months of taking the drug, I was in complete remission, and have remained so ever since.”
The drug, Velcade, was based on the Nobel Prize-winning work of Technion scientists Prof. Avram Hershko and Prof. Aaron Ciechanover (who became the founding Chairman of the Grand Center steering committee).
“When the Weizmann Institute approached us about supporting personalized medicine, the plan was always to build a national center—something that could bring together scientific and clinical research talent from all over the country, and, with the help of experts from industry, create targeted treatments that would benefit patients in Israel and beyond,” Stephen says. “It’s a new way to do biomedical science, and we are certain that over the long run, there will be great outcomes.”
“Genome science is creating a wide-open world of open possibilities, because it allows you to look at the building blocks of life, identify the source of medical problems, and also find solutions. But to succeed, you need the best equipment, and the right people. That’s why Nancy and I were excited about putting this platform in place.”
The Grands’ philanthropy encompasses academic pursuits, Jewish causes, and social welfare. At the Weizmann Institute, they also established the Grand Center for Sensors and Security. In San Francisco, they established the Nancy & Stephen Grand Family House, which provides temporary lodging to low-income families of pediatric cancer patients, enabling them to remain near their children while they are undergoing treatment. The couple also founded the Jewish Cultural Center in Odessa, Ukraine—the same city from which Stephen’s father fled, thereby escaping the fate of so many victims of the Holocaust.
“My parents’ generation was very close to Israel, and my father—who was president of a local chapter of the American Technion Society—passed that down to me,” Stephen says. “That’s why it’s so meaningful for us to be involved in the Israel National Center for Personalized Medicine. We don’t call our support a gift; we call it an investment in Israel’s future.”
Crown Institute for Genomics
Modern genomic approaches are helping to solve some of medicine’s biggest puzzles, as tools that grew out of the Human Genome Project help reveal molecular “mugshots” associated with cancer, diabetes, infectious diseases, mental illness and other conditions. Genomic research informs and improves medical practice, by helping clinicians do a better job of matching individual patients with the therapies they need. This, in a nutshell, is the mission of the G-INCPM’s Crown Institute for Genomics.
The Crown Institute’s modular services include consultation and project design, sample preparation by type, sequencing services, and bioinformatics-based data analysis. Through collaboration with academics, members of the clinical community, and industrial experts, the Crown Institute promotes personalized medicine by helping research groups get answers to their scientific questions.
The Crown Institute was established through a gift from Lester and Renée Crown.
de Botton Institute for Protein Profiling
Protein profiling involves the identification of the full complement of proteins expressed in a particular tissue, under a specified set of conditions and at a particular time, making it the very foundation of personalized medicine. At the G-INCPM, these important scientific activities have a single address: the de Botton Institute for Protein Profiling.
At the de Botton Institute, mass spectrometry and other advanced technologies are used to provide comprehensive analysis of proteins in biological samples. Working closely with scientific teams from the Weizmann Institute and beyond, experts at the de Botton Institute can identify and quantify even low-abundance proteins in any type of mixture, and detect modifications that take place after the protein is “minted” based on DNA instructions.
The Protein Profiling Institute was established through the generosity of Miel de Botton. A clinical psychologist, art collector and singer-songwriter, Ms. de Botton studied law at Oxford University and psychology in Paris, where she worked as a clinical therapist and drug addiction counselor.
Ilana and Pascal Mantoux Institute for Bioinformatics
As tools evolve to allow biologists to gather ever-larger quantities of data, scientific experiments can only be fully analyzed through a platform that integrates computers, software tools, and databases. This is the essence of bioinformatics, and this is the mission of the Ilana and Pascal Mantoux Institute for Bioinformatics at the G-INCPM.
At the Mantoux Institute, experts in data science, mathematics, physics, biology, and software engineering help investigators answer their research questions. Working with Weizmann researchers, as well as physicians and scientists from other institutions, the Mantoux Institute provides bioinformatics support for proteomics, high-throughput screening, and genomic analysis.
The Mantoux Institute for Bioinformatics was established through the generosity of Pascal and Ilana Mantoux.
Maurice and Vivienne Wohl Institute for Drug Discovery
If searching for a needle in a haystack is considered difficult, consider the difficulty of searching for one medically useful molecule. This is the mission of the Maurice and Vivienne Wohl Institute for Drug Discovery at the G-INCPM.
Specializing in the design and execution of high throughput experiments, the Wohl Institute team designs and executes screening procedures for identifying molecules that, with further development, may provide the basis for new and useful medications.
The Wohl Institute’s capabilities rest on three pillars: a “library” of chemical compounds against which new molecules can be tested; the design of customized and automated testing procedures; and sophisticated software to analyze experimental data. Thanks to the outstanding technical infrastructure for molecular screening that is available at the G-INCPM, Weizmann investigators, as well as academics from other research institutions and pharmaceutical companies, rely on the Wohl Institute to move drug discovery forward.
The late Vivienne and Maurice Wohl, benefactors of the Wohl Institute, are remembered for their rich legacy of support for medical science, welfare, and education.
The Grand INCPM’s founding supporters are Nancy and Stephen Grand, Miel de Botton, Lester and Renée Crown, Ilana and Pascal Mantoux, the David and Fela Shapell Family Foundation, Maurice and Vivienne Wohl, and the Wolfson Family Charitable Trust.
Dr. Liran Shlush is supported by The Applebaum Foundation, Rising Tide Foundation, Steven B. Rubenstein Research Fund for Leukemia and Other Blood Disorders, The Felix and Silvia Schnur Endowment Fund in Stem Cell Research, David and Fela Shapell Family Foundation INCPM Fund for Preclinical Studies, The Morris & Ruth Wagner and Marek Sutkiewicz Laboratory for Cancer Research, and the European Research Council. Dr. Shlush is the incumbent of the Ruth and Louis Leland Career Development Chair.

Dr. Berta Strulovici

Inside the de Botton Institute for Protein Profiling

Renée and Lester Crown

Miel de Botton

Pascal and Ilana Mantoux
Vivienne and Maurice Wohl