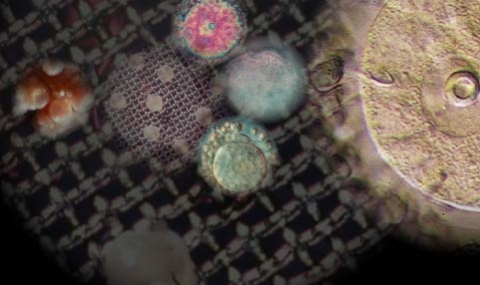
Oocyte meiosis in mammals is a protracted process, subject to several stop-go controls. The oocyte initiates the first meiotic division during embryonic life or shortly after birth. Meiosis is arrested, in most mammals, in neonatal life at diplotene/dictyate stage of the first meiotic prophase. The hallmark of the dictyate oocyte is the large nucleus known as “germinal vesicle” (GV).
During each reproductive cycle a number of oocytes, characteristic of the species, re-enter meiosis, manifested by germinal vesicle breakdown (GVBD). The first round of meiosis is completed with extrusion of the first polar body (PBI) and progress to the second meiotic metaphase. This resumption of meiosis and its progression to the metaphase of the second meiotic division is usually referred to as “oocyte maturation”. The meiotic process is arrested again (second meiotic arrest) and is completed, upon fertilization, by the extrusion of the second polar body (PBII). Oocyte maturation, as other ovulatory responses, is triggered by the pre-ovulatory surge of luteinizing hormone (LH).
The discrepancy between the spontaneous resumption of meiosis when oocytes were dislodged from their follicles, observed by Pincus and Enzmann already in 1935, and its dependence on LH-stimulation prompted us to establish a model for exploring the hormonal
stimulation of meiosis in vitro and reveal the pathways involved in the regulation of this process. This led to the development of the model of explanted rat pre-ovulatory follicles (or follicle-enclosed oocyte, FEO) allowing mechanistic studies meiosis (1,4). This model was adopted by many groups and significantly contributed to our present understanding of oocyte maturation and ovulation.
Using the FEO model we were able to evaluate the role of gonadotropins, cAMP, prostaglandins (4), steroidogenesis (10,12, 16) and aerobic glycolysis (13, 18) in the control of meiosis in mammals. These studies demonstrated the role of LH in triggering the resumption of meiosis and the mediatory role of cAMP in this process (Rev. 11 see details and contributions of Nava Dekel at Departmental site).
Reduction of oocyte cAMP levels is at the hub of resumption of meiosis. During a Sabbatical at Stanford, in collaboration with Marco Conti and Aaron Hsueh, we demonstrated differential regulation of phosphodiesterase (PDE) sub-types degrading cyclic nucleotides, like cAMP or cGMP, in the somatic cells of the follicle and the oocyte (118, 126, 132). Using milrinone or cilostamide, inhibiting the oocyte-specific PDE in the ovary, blocked LH-stimulated meiosis in vitro, as did the non-selective inhibitor isobutylmethylxanthine (IBMX). Conversely, rolipram inhibiting PDE4D in granulosa cells stimulated the maturation FEO, even without LH, presumably raising transiently follicular cAMP levels and mimicking LH effect. The oocyte-specific PDE type 3A has been shown to be upregulated by LH stimulation of FEO resulting in a decrease of oocyte cAMP levels allowing resumption of meiosis, while LH markedly stimulated cAMP production in the somatic compartment of the follicle (Rev. 133).
A most fundamental and surprising finding was the demonstration that in mammals, in stark contrast to lower vertebrates, steroids do not serve as the signal by which the somatic cells of the follicle transfer the gonadotropic stimulation of meiosis (16). We suggested that this might be associated with the hierarchical oocyte/follicle development in mammals and the resulting high levels of steroids usually present in the ovary and the follicle. This abundance presumably, precludes the use of steroids in mammals as a signal for the resumption of meiosis, as it is in amphibians and fishes (145, Rev. 146).
Oocyte meiosis in mammals is a protracted process, subject to several stop-go controls. The oocyte initiates the first meiotic division during embryonic life or shortly after birth. Meiosis is arrested, in most mammals, in neonatal life at diplotene/dictyate stage of the first meiotic prophase. The hallmark of the dictyate oocyte is the large nucleus known as “germinal vesicle” (GV).
During each reproductive cycle a number of oocytes, characteristic of the species, re-enter meiosis, manifested by germinal vesicle breakdown (GVBD). The first round of meiosis is completed with extrusion of the first polar body (PBI) and progress to the second meiotic metaphase. This resumption of meiosis and its progression to the metaphase of the second meiotic division is usually referred to as “oocyte maturation”. The meiotic process is arrested again (second meiotic arrest) and is completed, upon fertilization, by the extrusion of the second polar body (PBII). Oocyte maturation, as other ovulatory responses, is triggered by the pre-ovulatory surge of luteinizing hormone (LH).
The discrepancy between the spontaneous resumption of meiosis when oocytes were dislodged from their follicles, observed by Pincus and Enzmann already in 1935, and its dependence on LH-stimulation prompted us to establish a model for exploring the hormonal
stimulation of meiosis in vitro and reveal the pathways involved in the regulation of this process. This led to the development of the model of explanted rat pre-ovulatory follicles (or follicle-enclosed oocyte, FEO) allowing mechanistic studies meiosis (1,4). This model was adopted by many groups and significantly contributed to our present understanding of oocyte maturation and ovulation.
Using the FEO model we were able to evaluate the role of gonadotropins, cAMP, prostaglandins (4), steroidogenesis (10,12, 16) and aerobic glycolysis (13, 18) in the control of meiosis in mammals. These studies demonstrated the role of LH in triggering the resumption of meiosis and the mediatory role of cAMP in this process (Rev. 11 see details and contributions of Nava Dekel at Departmental site).
Reduction of oocyte cAMP levels is at the hub of resumption of meiosis. During a Sabbatical at Stanford, in collaboration with Marco Conti and Aaron Hsueh, we demonstrated differential regulation of phosphodiesterase (PDE) sub-types degrading cyclic nucleotides, like cAMP or cGMP, in the somatic cells of the follicle and the oocyte (118, 126, 132). Using milrinone or cilostamide, inhibiting the oocyte-specific PDE in the ovary, blocked LH-stimulated meiosis in vitro, as did the non-selective inhibitor isobutylmethylxanthine (IBMX). Conversely, rolipram inhibiting PDE4D in granulosa cells stimulated the maturation FEO, even without LH, presumably raising transiently follicular cAMP levels and mimicking LH effect. The oocyte-specific PDE type 3A has been shown to be upregulated by LH stimulation of FEO resulting in a decrease of oocyte cAMP levels allowing resumption of meiosis, while LH markedly stimulated cAMP production in the somatic compartment of the follicle (Rev. 133).
A most fundamental and surprising finding was the demonstration that in mammals, in stark contrast to lower vertebrates, steroids do not serve as the signal by which the somatic cells of the follicle transfer the gonadotropic stimulation of meiosis (16). We suggested that this might be associated with the hierarchical oocyte/follicle development in mammals and the resulting high levels of steroids usually present in the ovary and the follicle. This abundance presumably, precludes the use of steroids in mammals as a signal for the resumption of meiosis, as it is in amphibians and fishes (145, Rev. 146).