Diabetes can raise respiratory risk
A new study reveals how high blood sugar makes lung infections worse, and possible reversal strategies
Briefs

Lung tissue of a diabetic mouse (right) contains fewer immune cells (small purple dots) than that of a non-diabetic animal (left). (Images from the Elinav lab)
Clinicians have known for decades that people with diabetes are at a substantially increased risk of developing severe lung disease if they become infected with viruses such as influenza, as well as bacteria and fungi. When the COVID-19 pandemic erupted in early 2020, this mysterious phenomenon gained even more pressing importance: It became clear that people with diabetes were at a significantly higher risk of contracting severe, even fatal, lung disease after serious SARS-CoV-2 infection, but no one understood why. In fact, some 35% of people with COVID-19 who died during the pandemic had diabetes.
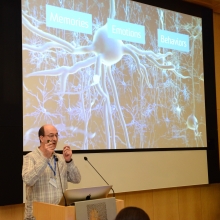
Research conducted at the Weizmann Institute and published in Nature in December 2023 has revealed how high levels of blood sugar in people with diabetes disrupt the function of key lung cell types that regulate the immune response. Led by Prof. Eran Elinav from the Department of Systems Immunology, the study’s authors also identified a potential strategy for reversing this susceptibility and saving lives.
The Elinav group exposed multiple mouse models of types 1 and 2 diabetes to a variety of viral lung infections. Just like humans with diabetes, the diabetic mice developed severe, fatal lung infections following exposure to lung pathogens such as influenza. The immune reaction, which in nondiabetics neutralizes the infection and drives tissue healing, was severely impaired in the diabetic mice, leading to uncontrolled infection, lung damage, and eventual death.
To decode the basis of this heightened risk, the researchers evaluated gene expression and immune and metabolic activity in over 150,000 individual lung cells from infected mice, both diabetic and nondiabetic. In the diabetic mice, they observed dysfunction in certain lung dendritic cells—the immune cells that orchestrate a targeted immune response against pathogenic infection. With these gatekeepers taken out of commission, the infection raged on unchecked.
Notably, the scientists discovered how high sugar levels in diabetic mice disrupt the normal function of lung dendritic cells during infection. Altered sugar metabolism in these cells led to the accumulation of metabolic byproducts that markedly disrupted the normal regulation of gene expression, leading to aberrant immune protein production.
Can the harmful effects of high sugar levels be prevented? The answer is yes: When the scientists administered supplemental insulin to control blood-sugar levels, the lung dendritic cells regained their capacity to generate a protective immune response that could prevent the cascade of events leading to a severe, life-threatening viral lung infection. Alternatively, administering small molecules to reverse the sugar-induced regulatory impairment corrected the dendritic cells’ dysfunction and enabled them to generate a protective immune response despite high sugar levels.
With over 500 million people worldwide affected by diabetes, a figure expected to rise in the coming decades, the Elinav group’s new research has significant, promising clinical implications. It may be possible to block diabetes-heightened risk for viral lung infection—and the devastating consequences.
“Our findings provide, for the first time, an explanation as to why diabetics are more susceptible to respiratory infection,” Prof. Elinav says. “Controlling sugar levels may make it possible to reduce this pronounced diabetes-associated risk. In diabetic patients whose sugar levels are not easily normalized, small molecule drugs may correct the gene alterations caused by high sugar levels, potentially alleviating or even preventing severe lung infection. Local administration of such treatments by inhalation may minimize adverse effects while enhancing effectiveness, and merits future human clinical testing.”
ERAN ELINAV IS SUPPORTED BY:
- Miel de Botton
- Leona M. and Harry B. Helmsley Charitable Trust
- Belle S. and Irving E. Meller Center for the Biology of Aging
- Rising Tide Foundation
- Mike and Valeria Rosenbloom Foundation
- Sagol Institute for Longevity Research
- Sagol Weizmann-MIT Bridge Program
- Sagol Center for Research on the Aging Brain
- Swiss Society Institute for Cancer Prevention Research
- Sir Marc and Lady Tania Feldmann Professorial Chair of Immunology
- The Vera Rosenberg Schwartz Research Fellow Chair supports a Staff Scientist in Prof. Elinav’s lab