In COVID-19, why does vulnerability rise with age?
The nature of senescent cells may hold the clue
Briefs

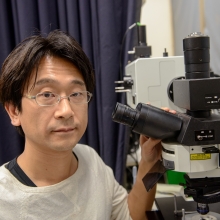
The world medical community is gasping for additional ventilators—machines that move air in and out of the lungs of COVID-19 patients who are having trouble breathing on their own. But what is it about the lungs of an individual that makes his or her respiratory system more vulnerable to coronavirus infection? And why does this vulnerability increase with age? The research of Prof. Valery Krizhanovsky, an expert in a unique stage of the cellular life cycle called senescence, may provide better answers to both of these questions.
Senescence is a “zombie-like” state in which cells permanently stop dividing, yet don’t die. The natural build-up of senescent cells—something akin to biological garbage that hasn’t been taken out—is a hallmark of aging tissues. It is also associated with a number of age-related diseases, including cancer.
In the early 2000s, the SARS (severe acute respiratory syndrome) virus began to spread all over the world. Caused by a coronavirus—the same family of viruses behind the current pandemic—SARS attacked through the lining of the lung, causing fever, shortness of breath, and pneumonia.
At that time, scientists demonstrated that the SARS virus enters the lungs by docking at a molecular receptor called angiotensin converting enzyme 2, or ACE2. Further, they showed that the more ACE2 a particular cell expressed, the more likely it was to become infected.
This is where Prof. Krizhanovsky, a member of the Weizmann Institute’s Department of Molecular Cell Biology, enters the story.
Prof. Krizhanovsky believes that increased presence of senescent cells—cells that have lost the ability to divide—in the lungs of elderly individuals may be a factor that drives high mortality among older COVID-19 patients. His hypothesis is based on compelling circumstantial evidence: AT2 cells, the sub-population of cells in the lung most likely to become senescent, express the coronavirus-binding ACE2 receptor at particularly high levels.
He suspects that—in addition to the “open door” to the coronavirus created by the ACE2 receptor—senescent cells may produce inhibitory molecules that disrupt the immune system’s protective activity. He is currently examining the correlation between ACE2 expression and senescence, to determine whether coronavirus-infected senescent lung cells have an edge in evading the body’s immune response.
This basic research may have important implications for practical therapeutics. If ACE2-rich senescent cells are indeed an “on ramp” that expedites coronavirus infection, it may be possible to use drugs to reduce the number of senescent cells. Such a treatment would reduce the overall viral load, leading to a more hopeful prognosis for COVID-19 patients, particularly the elderly.
Prof. Krizhanovsky is supported by Marlene and Bruce Kanter, the Ilse Katz Institute for Material Sciences and Magnetic Resonance Research, the Jeanne and Joseph Nissim Center for Life Sciences Research, Quinquin Foundation, Rising Tide Foundation, the Sagol Institute for Longevity Research, and the European Research Council. He is the incumbent of the Georg F. Duckwitz Professorial Chair of Cancer Research.
Prof. Valery Krizhanovsky