Brain-saving technology
New device combines algorithms, infrared light, and imaging to monitor bleeding in the brain
Features
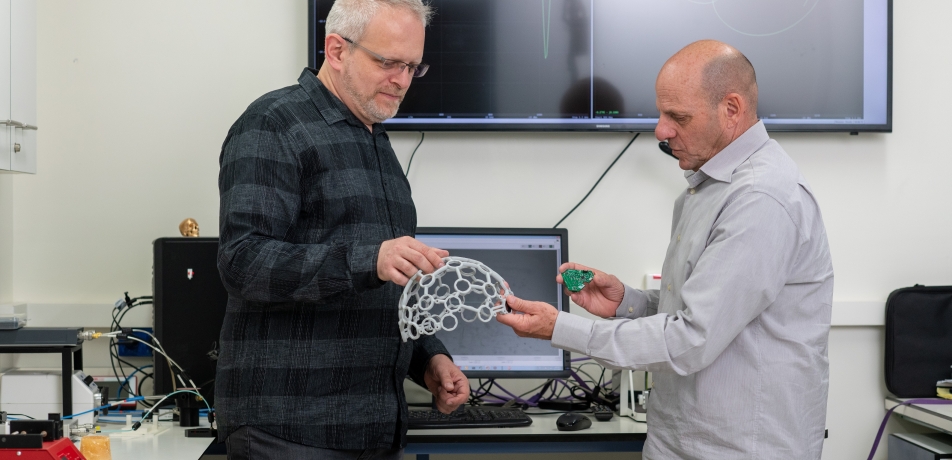
TOVA's inventors, L to R: Dr. Slava Kalchenko and Prof. Alon Harmelin
Imagine a physician peering into a patient’s head—from miles away—and diagnosing impending brain damage from an expanding blood clot, by simply glancing at a mobile device. That ability is close at hand, thanks to a collaboration between Prof. Alon Harmelin, Vice President for Administration and Finance; Dr. Slava Kalchenko, a senior staff scientist and Head of the In Vivo Optical Imaging Unit in the Department of Veterinary Resources at the Institute; and Dr. Paul Wright, a neurologist with Nuvance Health hospital network in New York State and Connecticut.
Prof. Harmelin and Dr. Kalchenko have developed an imaging system—called transcranial optical vascular assessment, or TOVA for short—that captures an image and data on the presence and growth of a subdural hematoma, a common type of bleeding within the skull on the outermost surface of the brain that frequently occurs after head injuries. TOVA comes in the form of a lightweight, wearable headgear connected wirelessly to a mobile device (such as a tablet or smart phone) for continuous, real-time monitoring via the cloud, along with a centralized monitoring system.
TOVA will be readily portable and designed for continuous use. Patients will receive the wearable headgear when they are discharged from a hospital or urgent care center, rather than undergo extended hospitalization and exposure to the ionizing radiation received from CT scan monitoring (the current method for diagnosing hematoma and other brain injuries). In this way, TOVA would offer an immediate reduction in the costs for prolonged hospitalizations while providing superior monitoring in one’s own home.
According to Prof. Harmelin, who developed the technology when he was head of the Department of Veterinary Resources, “TOVA will be a game-changer for how we treat head injuries.”
Casting a new light, using AI
The technological secret behind TOVA is a combination of infrared light and radiofrequency signals, coupled with sophisticated algorithms. It is based on a key scientific phenomenon where blood has measurably different light-absorption properties as it travels through different tissues in the cranium.
The idea behind using the light-absorption properties of blood to image the brain is more than 40 years old. However, the means for harnessing such properties in a way that is both sufficiently accurate and safe (radiation free) has been considered impossible—until now.
“The computational requirements for building the algorithms are quite complex,” says Dr. Kalchenko. “But thanks to the revolution in artificial intelligence-based ‘machine learning’ in the past 10 years, this is now possible.”
Prof. Harmelin and Dr. Kalchenko created an algorithm that can encode the blood/light ‘signature’ of a hematoma in various tissues, and can distinguish it from healthy brain tissue. That is, they built the algorithm using an AI ‘machine-learning’ technique involving a series of datasets that simulate different signatures, and then ‘taught’ these simulations to a computer program that could then distinguish the presence and size of a hematoma in live animal models.
And now, in collaboration with Dr. Paul Wright, Prof. Harmelin and Dr. Kalchenko are advancing the applicability and availability of this wearable headgear to the medical community.
This development comes at an important time. Thanks to medical advances that promote longevity, more and more people are living longer lives; an unintended consequence, however, is that more and more of them are on blood thinners due to cardiac disease.
“The elderly are more prone to falls, and if they fall while on blood thinners, there’s a high risk of having a traumatic brain bleed,” says Dr. Wright. “Even if the blood is drained away, there’s always a chance of a recurrence, which can go undetected until the next CT scan. Because TOVA offers real-time monitoring, the chances of significant brain injury are reduced.”
TOVA is able to scan to a depth of 3 cm into the brain, a relatively short distance. In this way, the technology fits a particular diagnostic niche, complementary to CT and MRI.
The goal is to make TOVA available in ambulances, doctor’s offices, and nursing homes. Even integration into motorcycle helmets and military headgear, for on-scene triage, may be possible.
The development of TOVA technology received support from business development experts at Yeda, the Weizmann Institute’s technology transfer arm, and its Innovation Development, Enhancement, and Acceleration (IDEA) program. IDEA is a new initiative to help Weizmann scientists bridge the gap between academia and industry. With Yeda’s help, TOVA will soon be on hand—and on head—wherever the patient is.
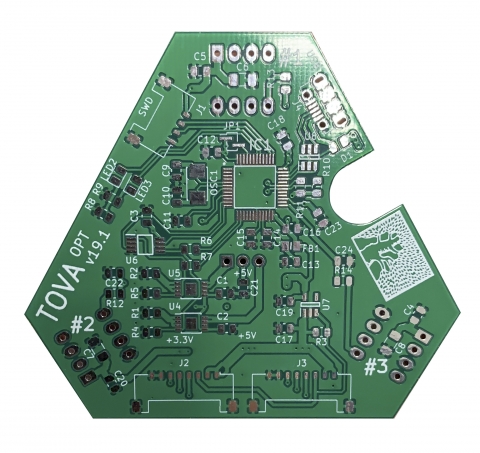
The TOVA chip








