Publications
Steffen Jung's complete bibliography
2005
-
(2005) Journal of Immunology. 175, 10, p. 6428-6435 Abstract
The peripheral lymphocyte pool size is governed by homeostatic mechanisms. Thus, grafted T cells expand and replenish T cell compartments in lymphopenic hosts. Lymphopenia-driven proliferation of naive CD8+ T cells depends on self-peptide/MHC class I complexes and the cytokine IL-7. Lymphopenia-driven proliferation and maintenance of memory CD8+ T cells are MHC independent, but are believed to require IL-7 and contact with a bone marrow-derived cell that presents the cytokine IL-15 by virtue of its high affinity receptor (IL-15Rα). In this study we show that optimal spontaneous proliferation of grafted naive and memory CD8+ T cells in mice rendered lymphopenic through gene ablation or irradiation requires the presence of CD11chigh dendritic cells. Our results suggest a dual role of CD11chigh dendritic cells as unique APC and cytokine-presenting cells.
(2005) Blood. 106, 9, p. 3004-3011 AbstractThe existence of macrophages (MΦ) of yolk-sac (YS) origin has been reported in all vertebrate models. However, the nature of their precursors and pathways of differentiation have not been elucidated. Phenotypic and differentiation potential analyses of YS at 7.5 to 10 postcoital days (dpc), performed in CX3CR1GFP embryos, allowed us to discern 3 independent MΦ populations. A first transient wave consisted of mature, maternal-derived MΦ present as early as 7.5 to 8 dpc. A second wave of committed MΦ precursors arose at 8 dpc (2-4 somite stage) and was followed by a third wave of erythromyeloid precursors (4-6 somite stage). Both types of precursors displayed similar phenotypes and gave rise to CX3CR1/green fluorescent protein (GFP)-positive MΦ, but differed by their differentiation potential, at the clonal level. The combined data of phenotypic, gene-expression, and in situ analyses allowed us to conclude that the previously named "primitive MΦ" corresponded to a mixture of the first transient wave and committed MΦ precursors. Both YS-derived precursors followed a developmental pathway common to adult MΦ and could be qualified as definitive.
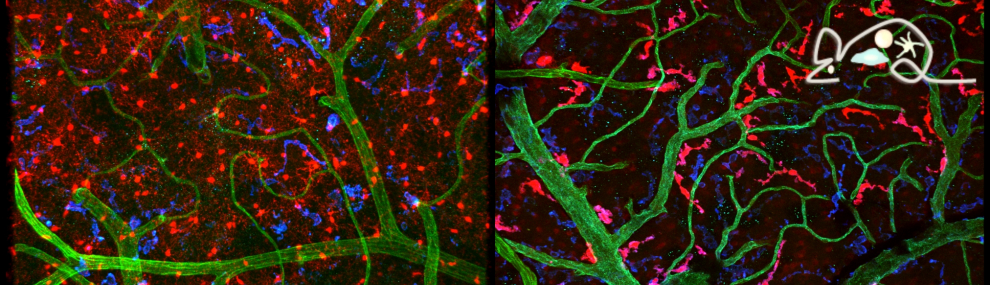
(2005) Nature Neuroscience. 8, 6, p. 752-758 AbstractParenchymal microglia are the principal immune cells of the brain. Time-lapse two-photon imaging of GFP-labeled microglia demonstrates that the fine termini of microglial processes are highly dynamic in the intact mouse cortex. Upon traumatic brain injury, microglial processes rapidly and autonomously converge on the site of injury without cell body movement, establishing a potential barrier between the healthy and injured tissue. This rapid chemotactic response can be mimicked by local injection of ATP and can be inhibited by the ATP-hydrolyzing enzyme apyrase or by blockers of G protein-coupled purinergic receptors and connexin channels, which are highly expressed in astrocytes. The baseline motility of microglial processes is also reduced significantly in the presence of apyrase and connexin channel inhibitors. Thus, extracellular ATP regulates microglial branch dynamics in the intact brain, and its release from the damaged tissue and surrounding astrocytes mediates a rapid microglial response towards injury.
(2005) Journal of Cell Biology. 169, 4, p. 569-576 AbstractLangerhans cells (LC) form a unique subset of dendritic cells (DC) in the epidermis but so far their in vivo functions in skin immunity and tolerance could not be determined, in particular in relation to dermal DC (dDC). Here, we exploit a novel diphtheria toxin (DT) receptor (DTR)/DT-based system to achieve inducible ablation of LC without affecting the skin environment. Within 24 h after intra-peritoneal injection of DT into Langerin-DTR mice LC are completely depleted from the epidermis and only begin to return 4 wk later. LC deletion occurs by apoptosis in the absence of inflammation and, in particular, the dDC compartment is not affected. In LC-depleted mice contact hypersensitivity (CHS) responses are significantly decreased, although ear swelling still occurs indicating that dDC can mediate CHS when necessary. Our results establish Langerin-DTR mice as a unique tool to study LC function in the steady state and to explore their relative importance compared with dDC in orchestrating skin immunity and tolerance.
(2005) European Journal of Immunology. 35, 5, p. 1463-1471 AbstractImmunization of mice with live or heat-killed Listeria monocytogenes (HKLM) efficiently primes pathogen-specific CD8+ T cells. T lymphocytes primed by HKLM, however, undergo attenuated proliferation and do not fully differentiate. Thus, only infection with live bacteria induces long-term, CD8+ T cell-mediated protective immunity. In this study we demonstrate that live and heat-killed bacteria, while both associating with Mac-3+CD11bhi cells, localize to distinct splenic areas following intravenous inoculation. While HKLM localize to the marginal zone and the splenic red pulp, live L. monocytogenes are carried to the T cell zone of splenic white pulp. Despite these differences, in vivo depletion of CD11c-expressing cells prevents priming of naive T cells by either HKLM or live L. monocytogenes. Analysis of CD11chi dendritic cells (DC) reveals that infection with live L. monocytogenes induces higher levels of CD40, CD80 and CD86 expression than immunization with HKLM. Our results suggest that CD8+ T cell priming following HKLM immunization or live infection is mediated by DC and that the disparate outcomes of priming can be attributed to suboptimal conditioning of DC in the absence of live, cytosol-invasive bacteria.
(2005) Journal of Experimental Medicine. 201, 6, p. 981-991 AbstractAlthough dendritic cells (DCs) play an important role in sensitization to inhaled allergens, their function in ongoing T helper (Th)2 cell-mediated eosinophilic airway inflammation underlying bronchial asthma is currently unknown. Here, we show in an ovalbumin (OVA)-driven murine asthma model that airway DCs acquire a mature phenotype and interact with CD4+ T cells within sites of peribronchial and perivascular inflammation. To study whether DCs contributed to inflammation, we depleted DCs from the airways of CD11c-diphtheria toxin (DT) receptor transgenic mice during the OVA aerosol challenge. Airway administration of DT depleted CD11c+ DCs and alveolar macrophages and abolished the characteristic features of asthma, including eosinophilic inflammation, goblet cell hyperplasia, and bronchial hyperreactivity. In the absence of CD11c+ cells, endogenous or adoptively transferred CD4+ Th2 cells did not produce interleukin (IL)-4, IL-5, and IL-13 in response to OVA aerosol. In CD11c-depleted mice, eosinophilic inflammation and Th2 cytokine secretion were restored by adoptive transfer of CD11c+ DCs, but not alveolar macrophages. These findings identify lung DCs as key proinflammatory cells that are necessary and sufficient for Th2 cell stimulation during ongoing airway inflammation.
(2005) Journal of Immunology. 175, 3, p. 1884-1893 Abstract[All authors]Mononuclear phagocytes enter the lungs both constitutively to maintain alveolar macrophage and dendritic cell homeostasis, as well as during lung inflammation, where the role of these cells is less well defined. We used a transgenic mouse strain (CX3CR1+/ GFP) that harbors a GFP label in circulating monocytes to identify and sort these cells from the vascular and alveolar compartments under both constitutive and acute lung inflammatory conditions. Using nylon arrays combined with real-time RT-PCR for gene expression profiling, we found that flow-sorted, highly purified mononuclear phagocytes recruited to acutely inflamed mouse lungs showed strongly up-regulated mRNA levels of the neutrophil chemoattractants KC, MIP-2, and IP-10, which contrasted with alveolar mononuclear phagocytes that immigrated in steady state. Similar observations were made for the lysosomal cathepsins B, L, and K being strongly up-regulated in mononuclear phagocytes upon recruitment to inflamed lungs but not during constitutive alveolar immigration. Inflammatory elicited mononuclear phagocytes also demonstrated significantly increased mRNA levels of the cytokine TNF-α and the PRR-associated molecules CD14, TLR4, and syndecan-4. Together, inflammatory elicited mononuclear phagocytes exhibit strongly increased neutrophil chemoattractants, lysosomal proteases, and LPS signaling mRNA transcripts, suggesting that these cells may play a major role in acute lung inflammatory processes.
(2005) Nature Methods. 2, 6, p. 419-426 AbstractA new system for lineage ablation is based on transgenic expression of a diphtheria toxin receptor (DTR) in mouse cells and application of diphtheria toxin (DT). To streamline this approach, we generated Cre-inducible DTR transgenic mice (iDTR) in which Cre-mediated excision of a STOP cassette renders cells sensitive to DT. We tested the iDTR strain by crossing to the T cell- and B cell-specific CD4-Cre and CD19-Cre strains, respectively, and observed efficient ablation of T and B cells after exposure to DT. In MOGi-Cre/iDTR double transgenic mice expressing Cre recombinase in oligodendrocytes, we observed myelin loss after intraperitoneal DT injections. Thus, DT crosses the blood-brain barrier and promotes cell ablation in the central nervous system. Notably, we show that the developing DT-specific antibody response is weak and not neutralizing, and thus does not impede the efficacy of DT. Our results validate the use of iDTR mice as a tool for cell ablation in vivo.
(2005) Science. 307, 5707, p. 254-258 Abstract[All authors]Dendritic cells (DCs) and macrophages are critical to innate and adaptive immunity to the intestinal bacterial microbiota. Here, we identify a myeloid-derived mucosal DC in mice, which populates the entire lamina propria of the small intestine. Lamina propria DCs were found to depend on the chemokine receptor CX3CR1 to form transepithelial dendrites, which enable the cells to directly sample luminal antigens. CX3CR1 was also found to control the clearance of entero-invasive pathogens by DCs. Thus, CX 3CR1-dependent processes, which control host interactions of specialized DCs with commensal and pathogenic bacteria, may regulate immunological tolerance and inflammation.
(2005) Nature Immunology. 6, 2, p. 198-203 AbstractTo become accessible for rearrangement, the immunoglobulin κ locus must undergo a series of epigenetic changes. This begins in pro-B cells with the relocation of both immunoglobulin κ alleles from the periphery to the center of the nucleus. In pre-B cells, one allele became preferentially packaged into an active chromatin structure characterized by histone acetylation and methylation of histone H3 lysine 4, while the other allele was recruited to heterochromatin, where it was associated with heterochromatin protein-γ and Ikaros. These events in cis made only one allele accessible to trans-acting factors, such as RelB, which mediated DNA demethylation, to facilitate rearrangement. These results suggest that early B lymphoid epigenetic changes generate differential structures that serve as the basis for allelic exclusion.